Can Colorectal Cancer Be Prevented?
There is no sure way to prevent colorectal cancer. But there are things you can do that might help lower your risk, such as changing the risk factors that you can control.
Colorectal cancer screening
Screening is the process of looking for cancer or pre-cancer in people who have no symptoms of the disease. Regular colorectal cancer screening is one of the most powerful weapons for preventing colorectal cancer.
From the time the first abnormal cells start to grow into polyps, it usually takes about 10 to 15 years for them to develop into colorectal cancer. With regular screening, most polyps can be found and removed before they have the chance to turn into cancer. Screening can also find colorectal cancer early, when it is highly curable.
Screening is recommended starting at age 50 for people who are not at increased risk of colorectal cancer. There are several different screening options available. People at higher risk, such as those with a strong family history of colorectal cancer, might benefit from starting screening at a younger age.
If you have a strong family history of colorectal polyps or cancer, talk with your doctor about your risk. You might benefit from genetic counseling to review your family medical tree to see how likely it is that you have a family cancer syndrome.
Body weight, physical activity, and diet
You might be able to lower your risk of colorectal cancer by managing some of the risk factors that you can control, like diet and physical activity.
Weight: Being overweight or obese increases the risk of colorectal cancer in both men and women, but the link seems to be stronger in men. Having more belly fat (that is, a larger waistline) has also been linked to colorectal cancer. Staying at a healthy weight and avoiding weight gain around the midsection may help lower your risk.
Physical activity: Increasing your level of activity lowers your risk of colorectal cancer and polyps. Regular moderate activity (doing things that make you breathe as hard as you would during a brisk walk) lowers the risk, but vigorous activity might have an even greater benefit. Increasing the intensity and amount of your physical activity may help reduce your risk.
Diet: Overall, diets that are high in vegetables, fruits, and whole grains (and low in red and processed meats) have been linked with lower colorectal cancer risk, although it’s not exactly clear which factors are important. Many studies have found a link between red meats (beef, pork, and lamb) or processed meats (such as hot dogs, sausage, and lunch meats) and increased colorectal cancer risk.Limiting red and processed meats and eating more vegetables and fruits may help lower your risk.
In recent years, some large studies have suggested that fiber in the diet, especially from whole grains, may lower colorectal cancer risk. Research in this area is still under way.
Alcohol: Several studies have found a higher risk of colorectal cancer with increased alcohol intake, especially among men.Avoiding excess alcohol may help reduce your risk.
For more about diet and physical activity, see the American Cancer Society Guidelines on Nutrition and Physical Activity for Cancer Prevention.
Not smoking
Long-term smoking is linked to an increased risk of colorectal cancer, as well as many other cancers and health problems.Quitting smoking may help lower you risk of colorectal cancer and other types of cancer. If you smoke and would like help quitting, call the American Cancer Society at 1-800-227-2345.
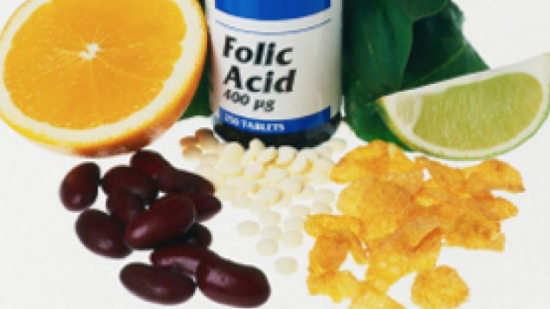
Vitamins, calcium, and magnesium
Some studies suggest that taking a daily multi-vitamin containing folic acid, or folate, may lower colorectal cancer risk, but not all studies have found this. In fact, some studies have hinted that folic acid might help existing tumors grow. More research is needed in this area.
Some studies have suggested that vitamin D, which you can get from sun exposure, in certain foods, or in a vitamin pill, might lower colorectal cancer risk. Because of concerns that excess sun exposure can cause skin cancer, most experts do not recommend this as a way to lower colorectal cancer risk at this time.More studies are needed to determine if vitamin D can help prevent colorectal cancer.
Low levels of dietary calcium have been linked with an increased risk of colorectal cancer in some studies. Other studies suggest that increasing calcium intake may lower colorectal cancer risk. Calcium is important for a number of health reasons aside from possible effects on cancer risk. But because of the possible increased risk of prostate cancer in men with high calcium intake, the American Cancer Society does not recommend increasing calcium intake specifically to try to lower colorectal cancer risk.
Calcium and vitamin D might work together to reduce colorectal cancer risk, as vitamin D aids in the body’s absorption of calcium. Still, not all studies have found that supplements of these nutrients reduce risk.
A few studies have found a possible link between a diet that is high in magnesium and reduced colorectal cancer risk, especially among women. More research is needed to determine if this link exists.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Many studies have found that people who regularly take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Motrin, Advil) and naproxen (Aleve), have a lower risk of colorectal cancer and polyps.
But aspirin and other NSAIDs can cause serious or even life-threatening side effects such as bleeding from stomach irritation or stomach ulcers, which may outweigh the benefits of these medicines for the general public. For this reason, most experts don’t recommend taking NSAIDs just to lower colorectal cancer risk if you are someone at average risk.
However, for some people in their 50s who have an elevated risk of heart disease, where low-dose aspirin is found to be beneficial, the aspirin may also have the added benefit of reducing the risk of colorectal cancer.
Because aspirin or other NSAIDs can have serious side effects, check with your doctor before starting any of them on a regular basis.
Hormone replacement therapy for women
Taking estrogen and progesterone after menopause (sometimes called menopausal hormone therapy or combined hormone replacement therapy) may reduce a woman’s risk of developing colorectal cancer, but cancers found in women taking these hormones after menopause may be at a more advanced stage.
Because taking estrogen and progesterone after menopause can also increase a woman’s risk of heart disease, blood clots, and cancers of the breast and lung, it is not commonly recommended just to lower colorectal cancer risk.
If you are considering using menopausal hormone therapy, be sure to discuss the pros and cons with your doctor.

The American Cancer Society medical and editorial content team
Our team is made up of doctors and master's-prepared nurses with deep knowledge of cancer care as well as journalists, editors, and translators with extensive experience in medical writing.